
Pulmonary Embolism Medical Failure to Diagnose Case in South Carolina
 We completed a case involving a failure to diagnose a pulmonary embolism (PE) in the emergency department of a major hospital. The failure to diagnose led to the death of a pregnant thirty year old woman.
We completed a case involving a failure to diagnose a pulmonary embolism (PE) in the emergency department of a major hospital. The failure to diagnose led to the death of a pregnant thirty year old woman.
A PE is a blood clot that travels to the lung, usually from the leg. The blood clot can cause obstruction of the blood flow in the lung and cause increased pressure on the right side of the heart. If the clot is large enough it can be fatal. Prompt diagnosis leads to the best outcome. Once diagnosed treatment consists of medications to “anti-coagulate” the patient so as to prevent more clot from forming. Once discovered, treatment of a blood clot with medications can be very effective.
The diagnosis of a PE can be challenging. The signs and symptoms can be very general and not specific to this particular condition. Some patients, but not all, may present with chest pain, shortness of breath (dyspnea), increased heart rate (tachycardia), increased respiratory rate (tachypnea); or coughing up blood (hemoptysis). The chest pain may be pleuritic in nature, meaning the patient may report pain with breathing. None of these signs or symptoms are diagnostic of a PE. A pregnant patient may have some of these findings simply by being pregnant. The key to an accurate diagnosis is for the clinician to have a high index of suspicion. Perhaps the most definitive test to rule out a PE is a CT angiogram (special type of x ray) or VQ perfusion scan (a special imaging study). However, not every patient with chest pain should get a CT angiogram to rule out a PE.
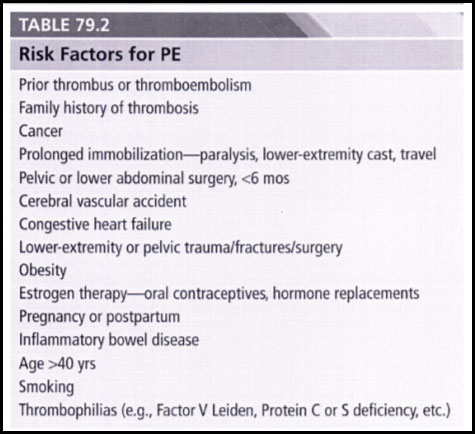
In evaluating a patient, physicians are concerned with the presence or absence of risk factors. In deciding whether to be suspicious for PE, a physician will look for established risk factors for the disease. Pregnancy is a known risk factor for PE. A positive family history is a known risk factor for PE.
Our client’s wife, a mother of two young children and ten weeks pregnant, presented to the emergency department. She had chest pain. It hurt when she took a breath. She was short of breath. Her respiratory rate was 40 bpm, way above normal. Her heart rate was elevated, at 110 bpm. The patient’s mother died from a PE.
The ER physician conducted a physical exam. He noted that the patient’s pain was “reproduced upon palpation”. That is, when he pressed in a certain area on her chest, the action caused the patient to experience pain. Reproduction of pain on palpation can be associated with benign muscular-skeletal complaints. Moreover, the doctor was impressed that her heart rate and respiratory rate decreased upon administration of morphine for pain control. The doctor performed an ultrasound of the right side of the heart and found a normal exam. Finally, the doctor was not impressed with the pleuritic chest pain, believing non-pleuritic pain had greater association with PE. Nor was he impressed with pregnancy and positive family history as risk factors. He concluded the patient had chest wall tenderness and sent her home. He ordered no CT angiogram. He ordered no anti-coagulation therapy. Nine days later the patient was dead from a massive PE.
Upon meeting this family, we realized how devasting these events were for the husband and his two young daughters. We decided quickly this was a case to investigate. During our work up of the case, studying the medical chart, reading the medical literature on pregnancy and PE, consulting with leading experts, and taking the depositions of the defense experts, we learned some very interesting things. We learned the ER physician made several key mistakes.
1) The ER doctor testified that pregnancy and positive family history were not risk factors for PE.
Our review of the literature showed just the opposite. See the chart below from the basic emergency medicine text, Harwood Nuss’ Clinical Practice of Emergency Medicine, 2015, listing risk factors for PE including Family history of thrombosis and Pregnancy or postpartum.
2) The ER physician testified pleuritic pain was not associated with PE
Again, our research of the medical literature found the opposite. Pleuritic chest pain is in fact associated with PE. See Amer Thoracic Society, Clinical Practice Guideline, May 2011. See Emergency Evaluation for Pulmonary Embolism Part 1, Clinical factors that increase risk. Kline. June 2015. “The clinical indications for imaging evaluation of suspected PE in pregnancy include, SOB, pleuritic chest pain, hypoxemia, tachycardia, to a lesser extent tachypnea, hemoptysis, syncope, cough, unexplained hypotension, other types of chest pain. (emphasis added).
3) The ER physician testified pain reproducible upon palpation reduced the likelihood of PE.
In certain instances reproducible pain can be an indication of a mere muscular skeletal problem. But the medical literature specifically cautions about using such a subjective method to rule out a PE. See Reproduction of chest pain by palpation: Diagnostic accuracy in suspected pulmonary embolism, British Medical Journal 2005. (“In patients with suspected pulmonary embolism, chest pain reproduced by palpation is not associated with a lower prevalence of pulmonary embolism…physicians should take into account that the usefulness of these widespread similogic descriptions may be limited in this situation”.) See Chest wall tenderness as a pitfall in the diagnosis of pulmonary embolism. A report of two cases. Arch Intern Med 1984. (“Clinicians should be alert to this mode of presentation and not exclude pulmonary embolism on the basis of such findings”.)
4) The ER doctor testified that normalization of vital signs argued against a PE.
In fact a leading expert in the field wrote just the opposite. See Normalization of Vital Signs Does Not reduce the Probability of Acute Pulmonary Embolism in Symptomatic Emergency Department Patients, Academic Emergency Medicine, Kline, 2012.
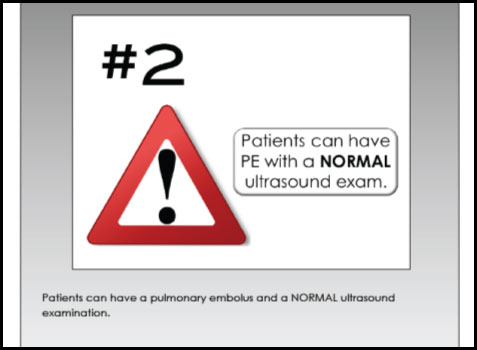
5) The ER doctor testified that a normal ultrasound of the right side of the heart reduced the likelihood of PE.
Through discovery, we determined the doctor’s own writings on the subject clearly demonstrated that a normal ultrasound could not rule out a small PE. The physician even had a powerpoint presentation with the following slide:
6) The ER physician testified that on the day of presentation to the emergency department the patient did not have a PE present that could have been diagnosed.
If true, this would be an excellent defense. If the condition is not present, then there is no way to diagnose the condition. Therefore, there is no way to miss the diagnosis. But was this true. During discovery we took the deposition of the defense experts hired by the defense. One admitted the patient possible had a PE on the day of presentation. The other testified she probably had the PE at time of presentation. Every expert in the case agreed that timely treatment with anti-coagulation would have prevented the death.
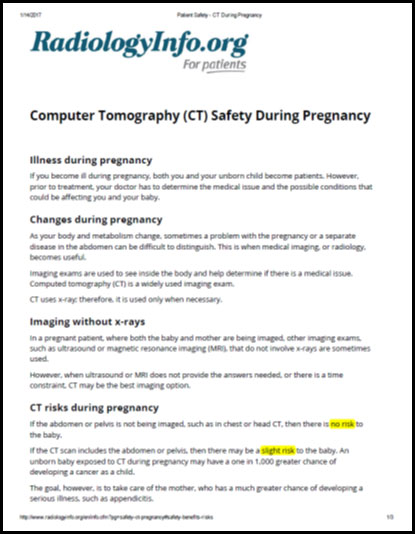
7) Finally, the ER physician testified that he would not have given the pregnant patient a CT angiogram because of the radiation risks to the unborn child. He would have to be really sure of a PE before subjecting a pregnant patient to this test.
This argument was badly undercut by the physician’s own expert witness who testified the radiation risk to the fetus of a CT angiogram to the chest was “negligible” and quite different from a CT angiogram to the abdomen. Our research confirmed this. We reviewed the web page of the radiologist who provided services to the emergency department. It had the following. Look at “CT risks during pregnancy”.
So, at the end of the day, we found the doctor wrong on many issues. His defense to the action was in tatters. We presented the follow:
The patient had at least two risk factors for PE and four signs/symptoms associated with PE. Therefore, PE needed to be on a differential diagnosis.
Potentially fatal conditions on a differential diagnosis need to be ruled out to promote patient safety. The most definitive test to rule out PE is a CTA. The risk of the test was negligible.
A CT angiogram would have found PE. PE is easily treated. The patient’s death was needless.
There were really only two conditions on the patient’s differential diagnosis: chest wall tenderness and PE. One is benign. One can kill if left untreated. The doctor convinced himself chest wall tenderness was more likely. Even if true, he still had to rule out PE. He didn’t.
The doctor gambled. He gambled the patient did not have a PE. He gambled with her health and was wrong. He gambled when he could have been sure. His gamble resulted in the death of two beings.
The case settled for $2.6 million.
Personal Injury Lawyers 1330 Laurel Street Columbia, SC 29201 Phone: 803-256-4242
Mailing Address
Post Office Box 1476
Columbia, South Carolina 29202
Fax: (803) 256-1952
Copyright © 2023 John D. Kassel, Attorney at Law, LLC. All rights reserved. Privacy Policy I Terms of Service | Disclaimer
This website is designed for general information only. The information should not be construed to constitute formal legal advice or the formation of a lawyer/client relationship. The results and testimonials listed on this website are specific to the facts and legal circumstances of specific cases and should not be used to form an expectation that the same results could be obtained for other clients in similar matters. This list is not a description or characterization of the quality of the firm's representation, it is not intended to compare one attorney's work to another and is in no way a guarantee of a specific result for your case.
